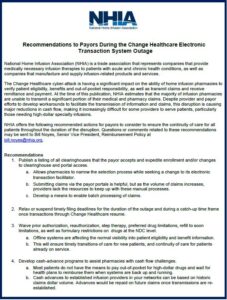
NHIA Releases 2024 Commercial Payor Recommendations
The National Home Infusion Association (NHIA) has developed recommendations for commercial, Medicaid, and Medicare Advantage payors to improve patient outcomes and experience, reduce administrative burden, and improve timely access to home infusion services.