Menu
Patient Stories
>
Fighting for Independence: Shane becomes advocate for same access to home infusion he values
By Jeannie Counce
Independence is highly valued among patients with chronic medical conditions, and home infusion therapy plays a significant role in supporting that independence. Having the flexibility to receive infusion therapy at home is important and, for those who self-administer, it offers a sense of control. Unfortunately, changes in coverage policies and unpredictable fluctuations in out-of-pocket costs can introduce barriers and create uncertainty, turning many patients into advocates.
“The people who are coming up with these policies don’t understand how it works for us,” says Shane Bare, a paraplegic patient with chronic inflammatory demyelinating polyneuropathy (CIDP) who relies on immune globulin (lg) to keep his disease at bay and remain mobile. In 2020, while he was appealing a coverage decision that resulted in out-of-pocket expenses upwards of $10,000/ month, Bare went off his therapy. “Once they stopped giving me my medicine, my symptoms came back right away but magnified. I’m already a paraplegic, if I lost my upper body, I’d be a vegetable. We were preparing for a funeral until we won the appeal.”
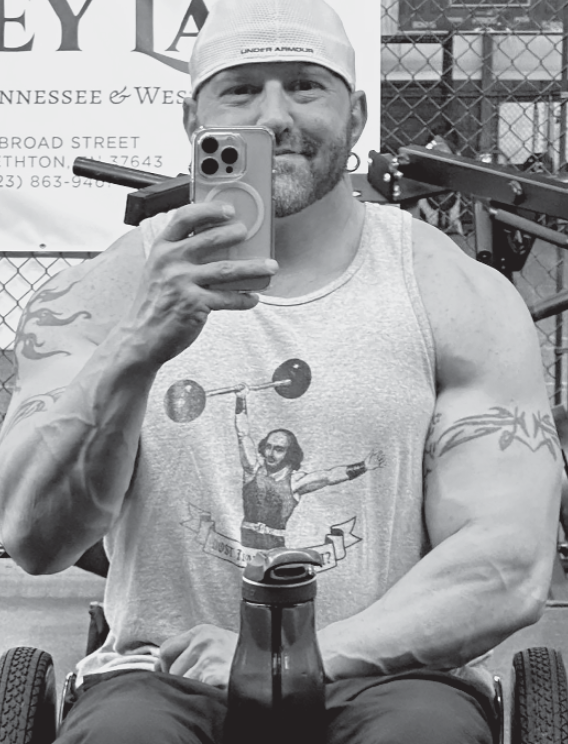
That was Bare’s first experience with advocacy. This summer, he joined a delegation of patients and NHIA leaders to Washington, DC to meet with members of Congress and officials at the Centers for Medicare and Medicaid Services (CMS) to promote comprehensive Medicare coverage of home infusion therapy. “l would like for the kind of thing that happened to me not to happen to other people—especially those people who don’t know that they can fight, or don’t know how,” he says.
Bare’s accesses to lg therapy is through a precarious patchwork of coverage and benefits that he fears are vulnerable to policy changes. He’s a Medicare beneficiary due to disability caused by a car accident 12 years ago. The lg formulation he takes, which is prescribed off-label, is covered by Medicare Part D and the related expenses are paid through patient assistance programs based on income. He doesn’t qualify for Medicaid and can’t find an affordable supplemental plan that would significantly reduce his out-of-pocket costs. “If the FDA approves my current formulation for CIDP and Medicare moves the coverage to Part B, I could be facing the same problem again,” he explains.

That’s why he joined NHIA in making the point to policymakers that patients need stable and sufficient coverage to ensure continued access to life-saving treatments. “l just want to know that I can get the therapy that keeps me healthy and active,” he says, noting that not every lg formulation works for every patient. In addition, Bare’s disability is contraindicated for intravenous (IV) lg, which further narrows his options. “My doctor says that subcutaneous (SC) administration is best for me because it reduces the risk of me developing blood clots. Also, I walk with my arms, so IV access isn’t a good idea,” he explains.
“l want to be as independent as I can,” says Bare, who self- administers SCIg once a week at home, which he says gives him the best quality of life. Although the therapy is effective, the initial medication onboarding makes him tired. “It knocks me out, so going to another location to get the infusion would be difficult. I’d need someone to drive me home. Loading up my chair and driving after infusion would be hard.”
By contrast, Bare feels completely comfortable managing his own therapy at home. “l like doing it by myself, on my own schedule—I have a routine,” he says. “When you do it all yourself, you have control. If something doesn’t feel right, you know it right away. You pay a lot closer attention because you don’t want to get it wrong.” In addition, home administration makes Bare less likely to miss a critical weekly dose due to travel logistics like not having a driver or inclement weather. “l can tell the further away I am from infusion day because I can feel the symptoms—little electrical shocks. I don’t want to miss a dose and go backwards.”
Bare says he was pleasantly surprised by the reception he and the others received in Washington. “They seemed receptive, and I hope they listened,” he says. “l wish I had more time with the CMS people because I had a whole folder of papers that I wanted to review with them,” he quips. “l really wanted them to understand how their decisions affect real people.”
Bare’s story highlights the need for comprehensive coverage of home infusion therapy and details its benefits in terms of patient well-being, cost-effectiveness, and efficient health care resource utilization. He contributed greatly to NHIA’s message to policymakers to ensure Medicare coverage for the full scope of home infusion services, consistent with the successful model employed by nearly every commercial plan.
“I’m glad we got the opportunity,” he says. “A lot of people are intimidated or take that denial letter as the final word instead of advocating for themselves.”

Jeannie Counce is the editorial director of NHIA. You can reach her at Jeannie.Counce@nhia.org
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |