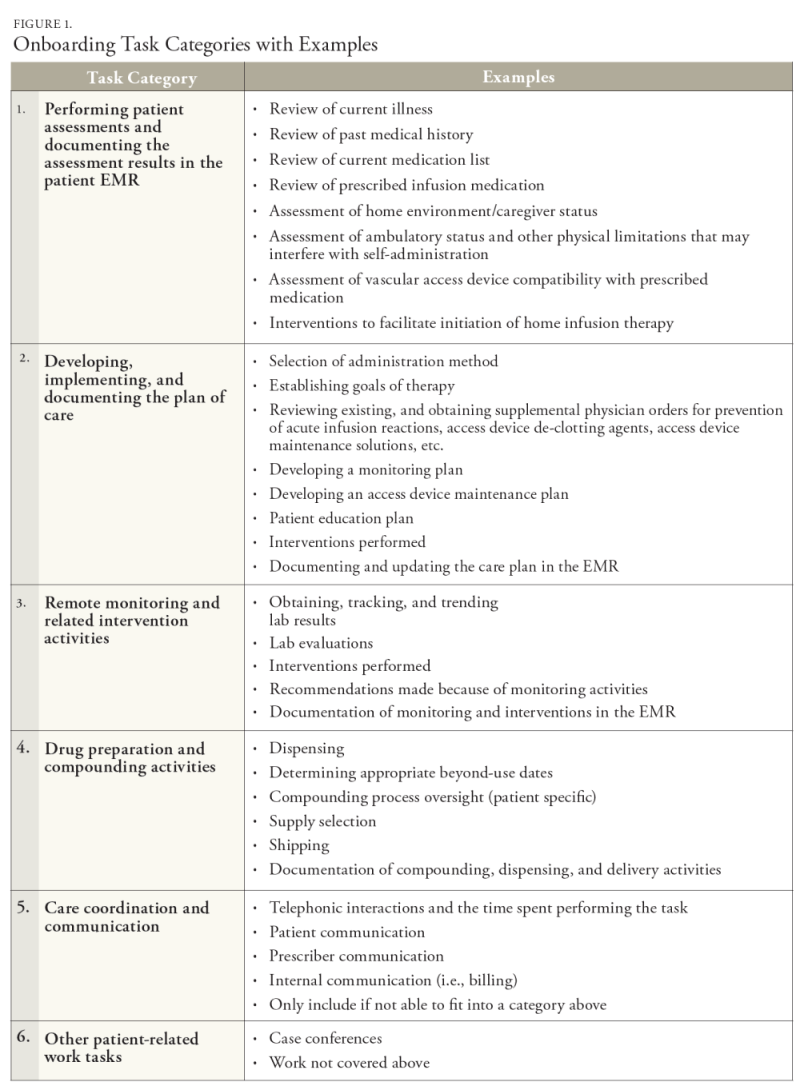
The home infusion patient onboarding process is essential to the patient’s success. It involves extensive multidisciplinary tasks that begin once the patient is referred for services. Onboarding is a term typically associated with newly hired employees and is the process by which employees gain the knowledge and skills they need to become effective members of an organization.1 Within health care, “patient onboarding” is a term typically used when the patient needs to be taught skills and knowledge prior to treatment. In the home infusion context, the term is broadened to include activities professional staff performs to arrange the home treatment. To ensure that the home infusion onboarding process is seamless, a team of infusion experts works simultaneously to determine patient eligibility, verify insurance coverage, design the therapy and monitoring plan, compound/ prepare the medications and supplies, establish treatment goals, and coordinate the home nursing services. The home infusion pharmacist performs a wide range of onboarding tasks, including consulting with the patient, physician, and nurse as needed and initiating changes to the prescribed treatment and monitoring plan.
For the pharmacist, the patient onboarding process is uniquely extensive, time-consuming, and inherently complex. The pharmacist must be knowledgeable of vascular access devices, infusion pumps, administration protocols and supplies, and maintain expertise in sterile compounding. Designing an effective infusion therapy requires adapting the prescribed medication to the individual patient’s needs and abilities while also considering the administration methods that are cost effective and suitable for the drug’s physical and chemical properties. Additionally, these functions are often completed in a short timeframe to facilitate an expeditious and seamless transition from hospital to home.
A review of the literature shows a void in studies focusing on pharmacist time to onboard a home infusion patient. Studies that investigate tasks and quantify the amount of time to complete are known as time utilization or time and motion studies. They are common in health care because they assist in understanding the time requirements specific to a health care profession.2 These studies were initially used to determine costs and inefficiencies in health care delivery and then expanded the focus toward patient safety and quality.2 Time utilization studies offer a precise standard in quantifying health care workers’ time expenditures on clinical activities and provide valuable insight into system specifications3 and workflow design.4 In brief, time utilization data is valuable for understanding the tasks required to provide a high-quality health care service efficiently.
There is a common understanding of the home infusion pharmacist’s professional contributions to onboarding the home infusion patient. However, the pharmacist’s overall time commitment to the various onboarding tasks is unknown. In 2022, the National Home Infusion Foundation (NHIF) conducted a time study that tracked 400 pharmacist tasks associated with 30 home infusion patients from 5 unique provider locations.5 The study concluded that pharmacists spend an average of 35.85 minutes per patient per day for an average of 12.23 study days per patient.5 However, this study did not delineate pharmacist onboarding tasks, or the amount of time or days needed to complete these tasks. A literature review shows that pharmacist time has been the main focus of some studies.3,6 Unfortunately, the investigations did not include home infusion pharmacy as the work setting and did not delineate onboarding time.
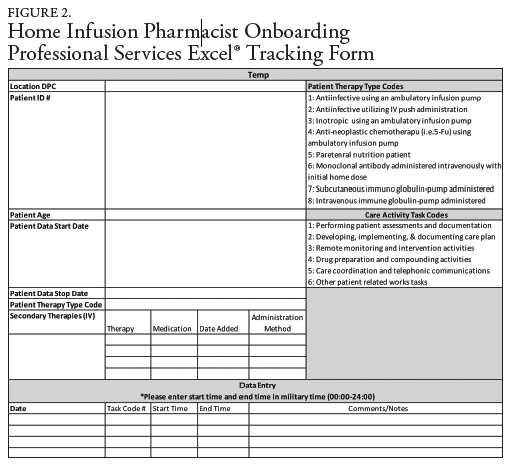
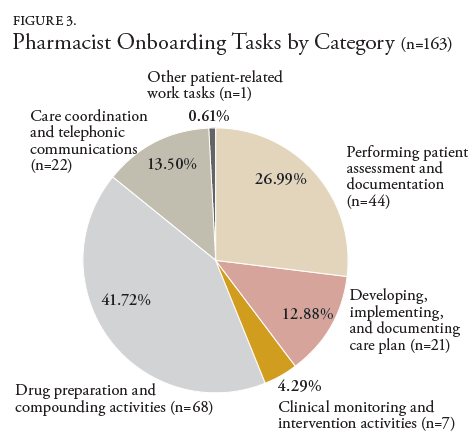
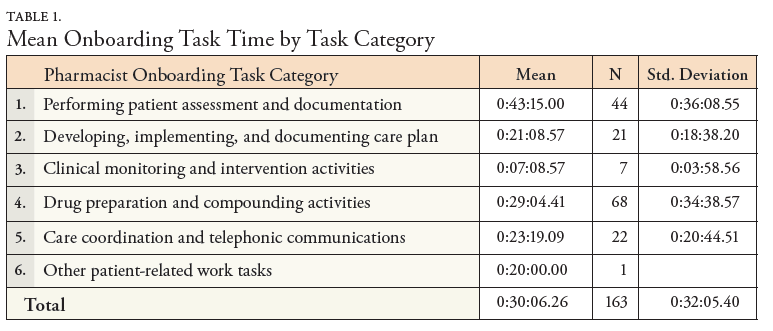
This multi-center descriptive study was conducted by NHIF to better understand the pharmacists work required to onboard a home infusion patient. The study objectives were to quantify the categories of professional services (tasks) the pharmacist provides, determine the amount of time the home infusion pharmacist spends onboarding the patient, and the number of days it takes to onboard a home infusion patient. This descriptive study will improve understanding of the type of work, amount of time, and number of days a pharmacist spends onboarding the home infusion patient.