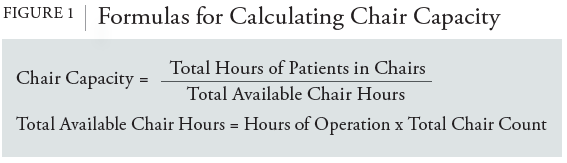
The simplicity of the theory behind chair capacity makes it an easy-to-use and easy-to-understand metric to show productivity. The total available chair-hours represent the theoretical maximum number of hours of infusions that the site can provide; if the site wished to offer more hours, it must increase the number of hours of its operations, add additional infusion chairs, or both. The optimal chair capacity that AIS sites strive to reach is as close to 100% as possible, to allow AIS sites to maximize the number of patients seen while minimizing vacancies between infusion appointments. However, it is generally not realistic to schedule patients such that when 1 patient arrives for an infusion, the person who had been occupying that specific chair will have just completed their appointment. According to the 2019 Infusion Center Volumes, Staffing, and Operations Survey, the median daily scheduled chair utilization rate was 80%, and the median actual chair utilization rate was 70%.4
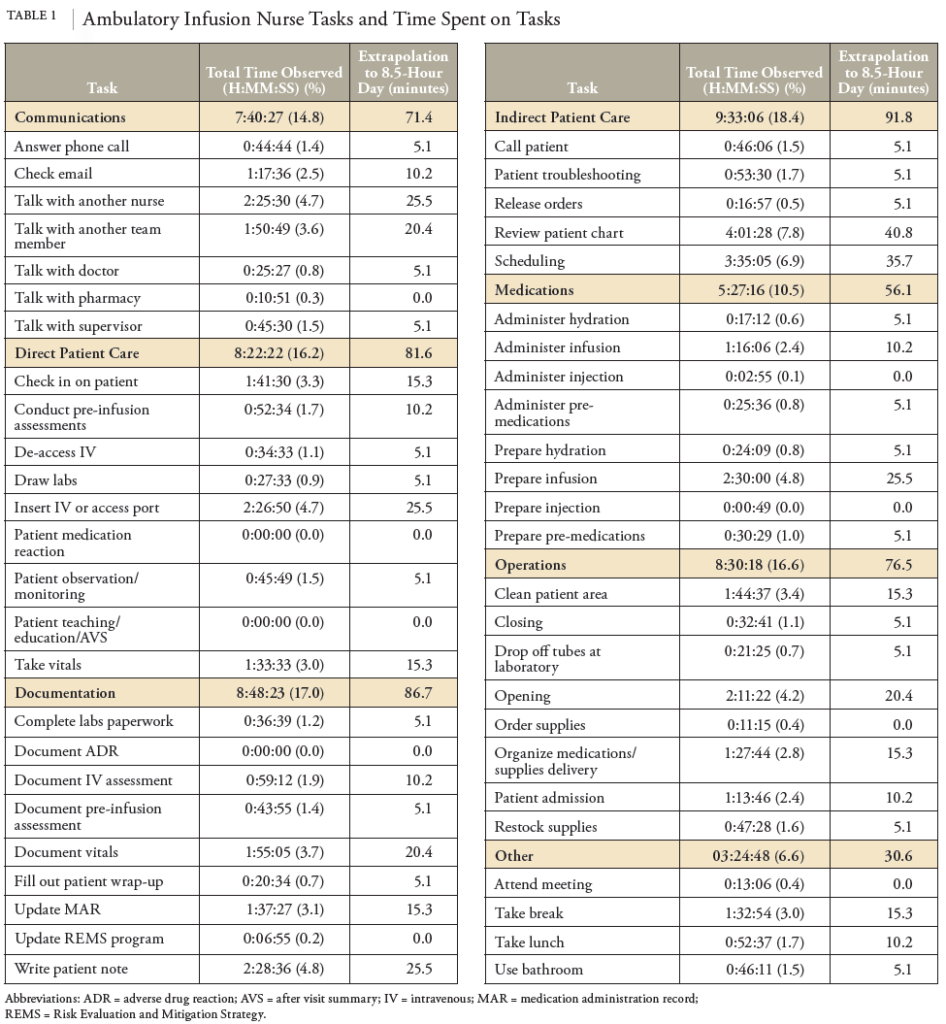
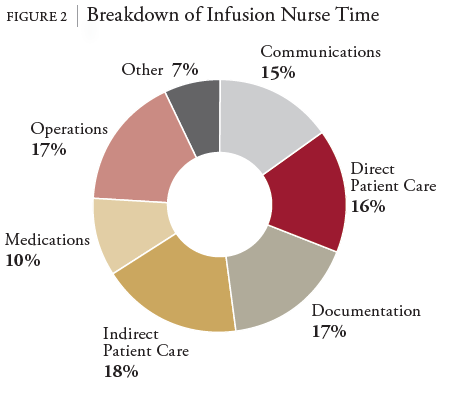
It is worth noting the drawbacks of chair capacity, even as it is the mainstay of AIS productivity measurement. First, chair capacity does not necessarily consider variability in the day. A full schedule may change because of appointment rescheduling, canceling, patient no-shows, or walk-ins. These changes may happen at any time and cannot easily be predicted. Although chair capacity would increase or decrease accordingly, it would not be able to provide an explanation on why the percentage was higher or lower than expected. Second, the sole number that chair occupancy presents can be misleading. The amount of time that a patient is sitting in an infusion chair may not necessarily equate to the amount of quality care they are receiving. Results of the 2014 National Hospital Oncology Benchmark for Infusion found that infusion chairs are utilized for active treatment only 18% of the total chair time available.5 Third, while it may seem that patients sit idly in infusion chairs for more than 80% of their time, it should be mentioned that infusion personnel, such as infusion nurses, are completing a multitude of tasks in the background. For example, infusion nurses are involved in communications, education, medication administration, and documentation, and they are often rapidly shifting between tasks or multitasking.6 Chair capacity gives no indication of this behind-the-scenes work. Thus, it is important to comprehend what is happening beyond the physical infusion chair.
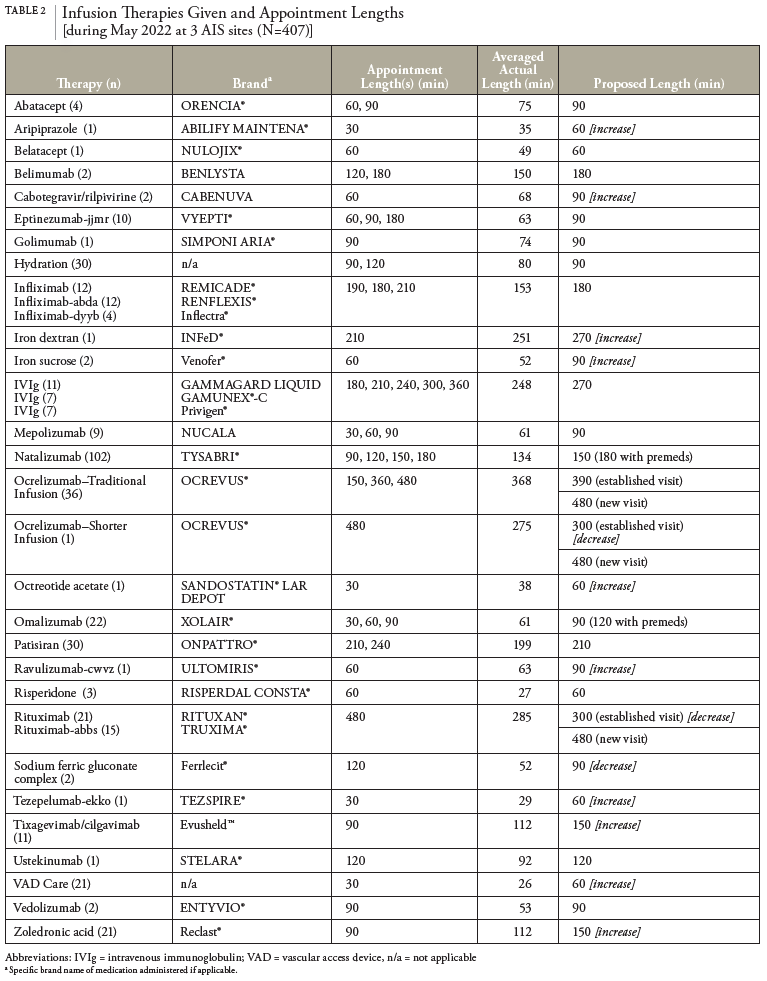
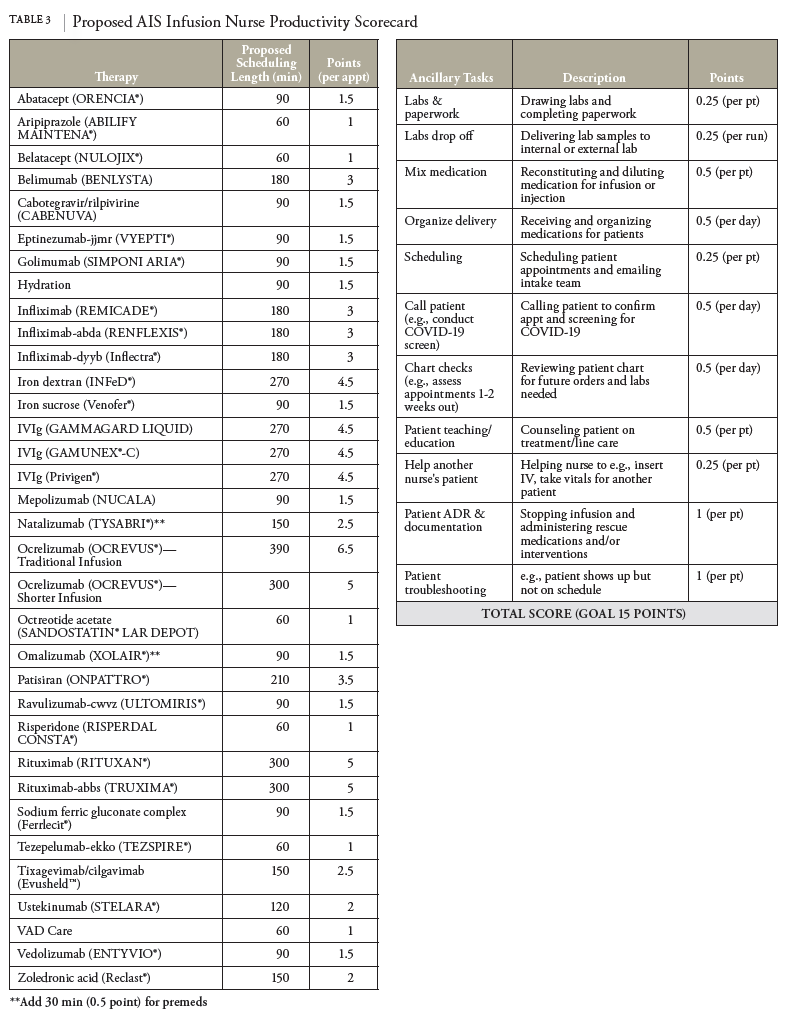
We argue that chair capacity’s ability to provide deeper insight into AIS operations and productivity is limited. We propose the need to pivot away from chair capacity to a different kind of metric, which we call “clinicianfocused capacity.” There is a need for metrics that can measure productivity not only more comprehensively, but also with an actionable level of detail. Instead of focusing on physical chair utilization, the focus should be on the infusion personnel who are orchestrating patient care and treatment. We believe that clinicianfocused capacity, which would measure productivity based on the tasks that infusion personnel spend their time on each day, would better inform AIS management on productivity. Clinician-focused capacity would paint a bigger picture of daily operations, as well as provide information to analyze where improvements in AIS site workflow can be made.
Unfortunately, minimal literature describes specific methods on how to collect data to measure productivity of infusion staff, not to mention standard metrics related to clinician-focused capacity. Some literature exists on the optimization of patient flow in infusion centers—specifically oncology infusion centers.7,8 However, there is minimal published literature that focuses on the workflow of infusion personnel. Additionally, there is little to no published literature on the study of workflow in non-oncology infusion suites.
Because of this lack of available information, we decided to develop a study to build out the concept of clinician-focused capacity. The intent of this project was to first identify a standardized set of tasks that can account for clinician-focused capacity, and in turn create an operational tool that AIS sites can use to inform productivity and business standards. Our goal was to provide a framework for AIS sites to use and begin incorporating clinician-focused capacity into their productivity metrics.
We note that this study specifically focused on developing clinician-focused capacity metrics with respect to infusion nurses. However, this study can be expanded to study other infusion personnel (e.g., pharmacists, pharmacy technicians, medical assistants) in the future.