1. National Home Infusion Association (NHIF). Infusion Industry Trends 2020. Alexandria, Va. NHIA 2020.
2. Polinski JM, Kowal MK, Gagnon M, Brennan TA, Shrank WH. Home infusion: Safe, clinically effective, patient preferred, and cost saving. Healthc (Amst). 2017 Mar;5(1-2):68-80. doi: 10.1016/j.hjdsi.2016.04.004. Epub 2016 Apr 29. PMID: 28668202.
3. HMP Global Learning Network. Research Reports, Pegfilgrastim Home Redirection Outcomes: Effectiveness and Timing of Administration in Primary Prophylaxis of Chemotherapy-Induced Neutropenia. Available at: https://www.hmpgloballearningnetwork.com/site/jcp/research-reports/pegfilgrastim-home-redirection-outcomes-effectiveness-and-timing (Accessed 26 July 2023).
4. UnitedHealth Group. Administering Specialty Drugs Outside Hospitals Can Improve Care and Reduce Costs by $4 Billion Each Year. Available at: https://www.unitedhealthgroup.com/content/dam/UHG/PDF/2019/UHG-Administered-Specialty-Drugs.pdf (Accessed 26 July 2023).
5. Psaltikidis EM, Silva END, Bustorff-Silva JM, Moretti ML, Resende MR. Economic evaluation of outpatient parenteral antimicrobial therapy: a systematic review. Expert Rev Pharmacoecon Outcomes Res. 2017 Aug;17(4):355-375. doi: 10.1080/14737167.2017.1360767. Epub 2017 Aug 4. PMID: 28776441
6. Balinsky W, Nesbitt S. Cost-effectiveness of outpatient parenteral antibiotics: a review of the literature. Am J Med. 1989 Sep;87(3):301-5. doi: 10.1016/s0002-9343(89)80155-x. PMID: 2505615.
7. Perraudin C, Bourdin A, Vicino A, Kuntzer T, Bugnon O, Berger J. Home-based subcutaneous immunoglobulin for chronic inflammatory demyelinating polyneuropathy patients: A Swiss cost-minimization analysis. PLoS One. 2020 Nov 25;15(11):e0242630. doi: 10.1371/journal.pone.0242630. PMID: 33237959; PMCID: PMC7688145.
8. Yong C, Fisher DA, Sklar GE, Li SC. A cost analysis of Outpatient Parenteral Antibiotic Therapy (OPAT): an Asian perspective. Int J Antimicrob Agents. 2009 Jan;33(1):46-51. doi: 10.1016/j.ijantimicag.2008.07.016. Epub 2008 Sep 26. PMID: 18823759.
9. Remonnay R, Devaux Y, Chauvin F, Dubost E, Carrère MO. Economic evaluation of antineoplasic chemotherapy administered at home or in hospitals. Int J Technol Assess Health Care. 2002 Summer;18(3):508-19. PMID: 12391944.
10. Thornton J, Elliott RA, Tully MP, Dodd M, Webb AK. Clinical and economic choices in the treatment of respiratory infections in cystic fibrosis: comparing hospital and home care. J Cyst Fibros. 2005 Dec;4(4):239-47. doi: 10.1016/j.jcf.2005.08.003. Epub 2005 Oct 19. PMID: 16242385.
11. Marshall JK, Gadowsky SL, Childs A, Armstrong D. Economic analysis of home vs hospital-based parenteral nutrition in Ontario, Canada. JPEN J Parenter Enteral Nutr. 2005 Jul-Aug;29(4):266-9. doi: 10.1177/0148607105029004266. PMID: 15961683.
12. Tsai TC, Doherty GM. Site of Care Optimization Through Home Hospital for Surgical Patients: The Next Frontier for Health Care Value and Population Health Management. Ann Surg. 2022 Jan 1;275(1):e278-e279. doi: 10.1097/SLA.0000000000005172. PMID: 34387212.
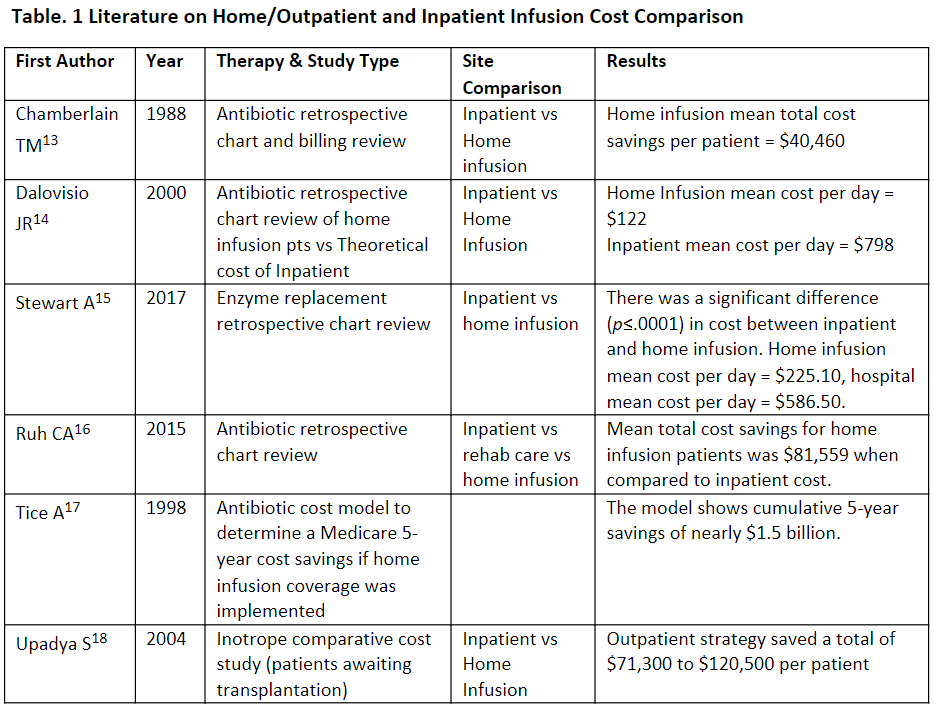
13. Chamberlain TM, Lehman ME, Groh MJ, Munroe WP, Reinders TP. Cost analysis of a home intravenous antibiotic program. Am J Hosp Pharm. 1988 Nov;45(11):2341-5. PMID: 3228090.
14. Dalovisio JR, Juneau J, Baumgarten K, Kateiva J. Financial impact of a home intravenous antibiotic program on a medicare managed care program. Clin Infect Dis. 2000 Apr;30(4):639-42. doi: 10.1086/313755. Epub 2000 Apr 4. PMID: 10770722.
15. Stewart, A., & Hao, L. (2017). Comparison Of Costs Between Hospital And Home Infusions In Patients Treated With Laronidase. Value in Health, 20(9), A496.
16. Ruh CA, Parameswaran GI, Wojciechowski AL, Mergenhagen KA. Outcomes and Pharmacoeconomic Analysis of a Home Intravenous Antibiotic Infusion Program in Veterans. Clin Ther. 2015 Nov 1;37(11):2527-35. doi: 10.1016/j.clinthera.2015.09.009. Epub 2015 Oct 21. PMID: 26471204.
17. Tice AD, Poretz D, Cook F, Zinner D, Strauss MJ. Medicare coverage of outpatient ambulatory intravenous antibiotic therapy: a program that pays for itself. Clin Infect Dis. 1998 Dec;27(6):1415-21. doi: 10.1086/515028. PMID: 9868653.
18. Upadya SP, Sedrakyan A, Saldarriaga C, Nystrom K, Bozzo J, Lee FA, Katz SD. Comparative costs of home positive inotropic infusion versus in-hospital care in patients awaiting cardiac transplantation. J Card Fail. 2004 Oct;10(5):384-9. doi: 10.1016/j.cardfail.2004.02.004. PMID: 15470648.
19. Home infusion therapy services. Centers for Medicare & Medicaid Services. Updated January 19, 2022. Accessed July 4, 2023. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Home-Infusion-Therapy/Overview#:~:text=Home%20infusion%20therapy%20 involves%20the,example%2C%20tubing%20and%20catheters
20. NHIA denounces CMS proposed home infusion rule. News release. National Home Infusion Association. July 12, 2019. Accessed July 4, 2023. https://nhia.org/documents/CMS_proposed_rule_press_release.pdf