Menu
October 5, 2021
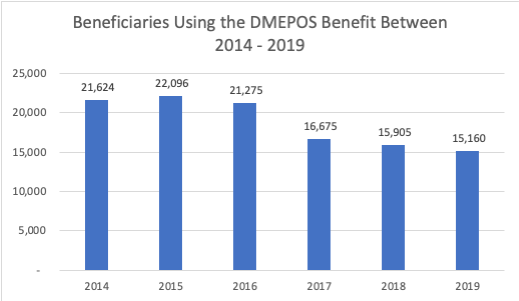
New publicly available data from the Centers for Medicare and Medicaid Services for CY 2019 shows that beneficiary utilization of the Part B DMEPOS home infusion benefit continued to decline despite the availability of the additional payment for nursing services under the transitional benefit.
NHIA believes the continued decline in utilization of home infusion for Part B covered therapies is evidence that CMS’s interpretation of “home infusion calendar day” is hurting Medicare beneficiaries and is insufficient to encourage provider participation in the program. Overall, the benefit utilization declined another 2% from prior year (2018) and provider participation in the program declined to the lowest point in 5 years. No services payments were available for 2017 and 2018, causing some to speculate the benefit might rebound once the add-on payment for services became available.
“Clearly, CMS’s gamble of limiting payment to face-to-face nursing has not paid off,” said NHIA President and CEO Connie Sullivan, BSPharm. “Over the past decade, private sector home infusion has experienced significant growth, largely due to an aging population and potential for cost-savings. Passing legislation to ensure proper recognition and payment for pharmacist services is critical to ensuring Medicare beneficiaries can continue to receive home infusion.”
Learn more about our current legislative efforts and how to get involved.
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |