Menu
The following references are now available as a NHIA member-only benefit and will redirect to our Community.
There are several reimbursement methodologies used to provide home infusion. This section will assist members in understanding these methodologies and knowing how to apply them to submit clean claims.
Please contact marianne.buehler@nhia.org if you have any questions or comments about the NHIA Reimbursement Training Center.
The NHIA Payer Advocacy and Relations Committee has created this NHIA resource to assist members in understanding the various reimbursement methodologies used to recognize the products and services provided to patient and how to translate them to a clean claim. You can click on the outline of topics below to jump direct to that section.
Home Infusion supplies and services can be billed to various parts of insurance programs called benefit types, which include the following.
Medical Benefit (Major Medical)
Pharmacy Benefit (Pharmacy Benefit Manager (PBM) and Medicare Part D)
Durable Medical Equipment (DME) Benefit
Home Health Benefit (Nursing)
Sometimes various services and supplies are billed to different benefits types, this is referred to as “Split Billing”.
The patient’s policy and payer requirements drive whether drugs are billed to the pharmacy benefit or the major medical benefit. This should be identified during the intake/beneift verification process.
Medical Benefit (Major Medical)
Drugs are generally billed using a combination of the HCPCS (Healthcare Common Procedure Coding System Level II codes) and the NDC (National Drug Code).
HCPCS codes are a unique, five-digit alpha numeric number; the first letter of a HCPCS code identifies which category the item or service falls into. Drug HCPCS Codes commonly begin with “J”. HCPCS descriptions provide the billable unit of a specific J-code. A single J code may be used to describe multiple strengths and/or manufacturers for the same drug.
To calculate the billable HCPCS units the amount dispensed is divided by the HCPCS unit value.
AMOUNT OF DISPENSED DRUG / HCPCS VALUE = UNITS BILLED*
*If the answer is a fraction, round up to the nearest whole HCPCS unit.
Example: Order for Ceftriaxone 2gm x 7 vials
- HCPCS Code for Ceftriaxone: J0696
- HCPCS Unit for Ceftriaxone: per 250 mg
To calculate HCPCS units for this order:
Multiply 7 vials x 2000mg (2gm) each vial = 14,000 mg total
Divide 14000mg / 250mg HCPCS unit = 56 HCPCS units
NDC codes uniquely identify each drug, including its manufacturer, strength, dosage form, formulation and package size. A single drug “name” may have multiple sizes, strengths and/or manufacturers, and as a result multiple NDC numbers. The billable unit is based on the specific “container” used (vial, bag, etc.).
Using the same example as above billing with NDC units:
7 vials = 7 units of the NDC
Other Considerations
Pharmacy Benefit (Pharmacy Benefit Manager (PBM) and Medicare Part D)
This method of billing is called National Council for Prescription Drug Programs (NCPDP) which refers to a national organization who has developed electronic standards for submitting Pharmacy Benefit Manager (PBM) drug claims.
NCPDP claims are billed using the NDC #, the NDC unit of measure, and number of units dispensed.
Example: Order for Ceftriaxone 2gm x 7 vials
To calculate NDC units for this order:
Multiply 7 vials dispensed x 1 NDC unit per vial = 7 NDC units .
Unlike HCPCS billing, NDC unit of measurement (UOM) billing does allow for fractions. Be sure to check with your manager regarding billing for partial vials. Example: if the pharmacy had used a 10GM vial of vancomycin but only dispensed 5GM, the units billed could be entered as 0.5 which would reflect the actual amount of drug dispensed.
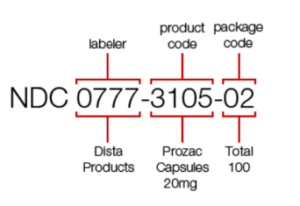
NDC Number
As indicated earlier, the NDC number is assigned to every drug and the numbers represent the manufacturer, the product and the package size. An NDC number consists of 3 sets of numbers. The first 5 digits are the manufacturer code, the second set of 4 numbers are the product code and the third set of 2 numbers reflect the package size.
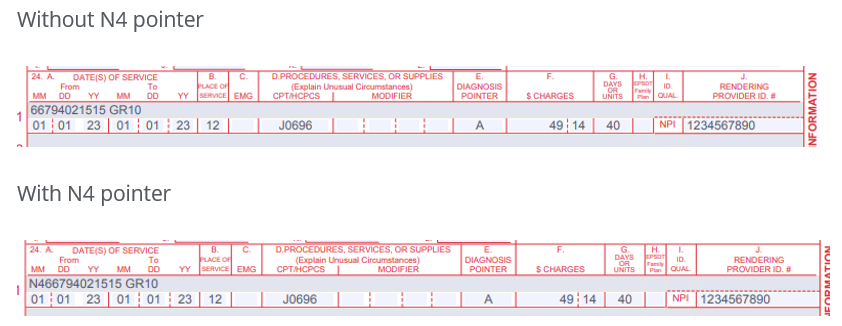
The NDC unit of measure (UOM) is entered in the red shaded portion of box 24 on the CMS 1500 form. The 11-digit number is entered without dashes, followed by the unit of measure and then the quantity.
It may be required to enter an N4 “pointer” before the NDC # to identify to the payer that you are billing a drug NDC #.
The NDC UOM is based on the original form of the drug which can likely be found on the inventory level of the provider’s billing software. In the examples below, the original form of ceftriaxone is a powder that must be reconstituted thus the NDC unit is UN.
Example: Ceftriaxone 2GM daily x 7 days, original form of the drug is a powder that must be reconstituted. HCPCS J0696 – Injection, ceftriaxone sodium, per 250 mg
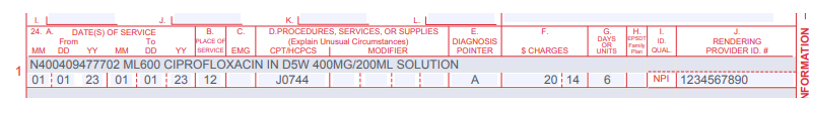
The original form of ciprofloxacin is a solution so the unit of measure is ML. The quantity billed is based on the total volume of the original form of the drug. In the example below, the original form is 400mg in 200ml of dextrose. The quantity billed for 3 doses is 600ml.
Example: Ciprofloxacin 400mg daily x 3 days, original form of the drug is a solution (400mg/200ml). HCPCS J0744 – Injection, ciprofloxacin for intravenous infusion, 200 mg. Total units billed is 6. 400mg times 3 days equals 1200mg total. 1200mg divided by the HCPCS unit of 200mg equals 6 units.
Drug Units of Measure (UOM)
| Common Drug Units of Measure (UOM) | |||
| UN | Unit – Powder for injection (needs to be reconstituted), pellet, kit, patch, tablet, device | ||
| ML | Milliliter – Liquid, solution, or suspension | ||
| GR | Gram – Ointments, creams, inhalers or bulk powder in a jar | ||
| F2 | International Unit – Products described as IU/vial or micrograms | ||
Drug Payment Methodologies
Drug payments methodologies vary from payer to payer, and are often based on the following:
ASP – Average Sales Price
AWP – Average Wholesale Price
MAC – Maximum Allowable Cost
WAC – Wholesale Acquisition Cost
FUL – Federal Upper Limit
NADAC – National Average Drug Acquisition Cost
There are two types of codes that are used to bill for home infusion services, supplies and equipment. Commercial payers have largely adopted per diem codes which bundle the supplies, equipment and many of the clinical services. Government payers typically use codes that are supply and/or pump driven and are often referred to as equipment and supply codes, A/E codes or Medicare kit codes, we will refer to them as equipment and supply codes.
Providers should look to the payer contracts for billable codes and allowances. In the absence of a contract, there may be guidance on the payer’s website in the form of fee schedules which may include the codes, allowances, and in some cases unit limitations.
Although the direction provided below reflects the industry standard, payer requirements may vary and must be followed to ensure correct payments.
Primary therapy: S9366 x one unit per day
Secondary therapy: S9500 SH x one unit per day
Tertiary therapy: S9351 SJ x one unit per day
Equipment and Supply Code Billing
Government payers may not recognize per diem S codes in which case the provider may utilize other code sets within HCPCS Level II. For purposes of distinguishing these codes from per diem codes, they will be referred to as Equipment and Supply codes. HCPCS begin with a letter that identifies the item type:
A – Supply Codes and Kit Codes
B – Enteral and Parenteral Nutrition (PN) Codes
E – Equipment Codes
E CODES – Equipment Codes
Durable Medical Equipment (DME) is defined as a piece of equipment that can withstand repeated use.
External Infusion Pump (EIP)
A mechanical pump is considered an item of durable medical equipment (DME). Payers typically have a monthly rental allowance, which may cap after a number of months rental. Most EIP, not used for Enteral or Parenteral Nutrition (PN) therapies, are billed with E0781 – Ambulatory infusion pump, single or multiple channels, electric or battery operated, with administrative equipment, worn by patient. E0781 is typically billed once per month on the anniversary date. Payers will likely require a reoccurring rental (RR) modifier indicating that it is a rental, modifiers may be required to designate the month of the rental. (KH=first month, KI=second and third month and KJ=the fourth through the 13th month). Payer policies should be consulted to determine limitations on the number of months that can be billed and as to whether pump ownership must be transferred to the patient after a certain number of rental months have been billed.
Syringe Pump
Therapies such as subcutaneous immunoglobulin require a syringe pump that allows for a prolonged infusion. The pump is bill with code E0779 – Ambulatory infusion pump, mechanical, reusable, for infusion 8 hours or greater. The modifier logic is the same as noted above for E0781. The supply code used in conjunction with E0779 is K0552 – Supplies for external non-insulin drug infusion pump, syringe type cartridge, sterile, each. K0552 is billed per container, in this case per syringe. Cath care supplies are not billed with a syringe pump because the infusion is subcutaneous (subQ) and there is not an access line that requires maintenance. When the infusion is complete, the subQ sets are removed.
IV Pole
An IV Pole (E0776) may be billable for stationary pumps. Some payer rent IV poles, while others purchase outright.
A CODES – Medical and Surgical Supplies
Codes that fall under this category are driven by quantity except for the code used for catheter care supplies. The number of infusion days is not a factor in determining units billed.
A4221: Catheter care supplies; may bill one unit per week/7 days, regardless of the number of supplies
A4222: Supplies used with an external infusion pump (EIP); units billed equals the number of containers.
Examples: 4 cassettes of an antibiotic, 2 bags of an inotrope
A4223: Supplies used when there is NOT an EIP. Units billed equals the number of containers.
Examples: 10 bags of hydration, 21 doses of an antibiotic in an elastomeric, 12 IV antibiotic piggybacks
Elastomerics
An elastomeric is a type of container that is used to dispense drugs. This is often called a non-mechanical pump or disposable pump, but it should not be confused with DME (durable medical equipment). There are two codes for the elastomerics which are based on the flow rate of the device.
A4305: elastomeric with a flow rate of 50ml or more per hour
A4306: elastomeric with a flow rate of less than 50ml per hour
Like the supply codes noted above, units are billed based on the number of containers. Payer policies should be reviewed to determine if these codes are payable with A4223 or whether there is an allowance or unit limitations.
While not an A code K0552 is a supply code used for infused drugs.
K0552: a temporary code used by the DME MAC and is exclusively used for syringe pump supplies. Units billed are determined by the number of syringes dispensed.
B CODES – Nutrition Support Therapy
Enteral and parenteral nutrition support therapies consist of medical treatment necessary to maintain or restore optimal nutrition status and health. Pumps, supplies (often in the form of kits), and nutrients are billed using the following codes. Note: Kits are a daily allowance of supplies for each day nutrients are delivered.
Enteral Pump Billing
B9002: Enteral nutrition with or without alarm
Enteral Kit Codes
B4034: Syringe/bolus fed
B4035: Pump fed
B4036: Gravity fed
Feeding Tubes (may be covered in addition to the kit)
B4081: NASOGASTRIC TUBING WITH STYLET B4082: NASOGASTRIC TUBING WITHOUT STYLET B4083: STOMACH TUBE – LEVINE TYPE B4087: GASTROSTOMY/JEJUNOSTOMY TUBE, STANDARD B4088: GASTROSTOMY/JEJUNOSTOMY TUBE, LOW-PROFILE
Enteral Formulas
There are about a dozen different enteral formula codes, all of which are billed with a unit of 100 calories.
| Enteral Formula (EF) B-Codes | ||
| HCPCS Code | Description | Billing Unit |
| B4149 | EF blenderized foods | 1 unit = 100 calories |
| B4150 | EF complet w/intact nutrient | 1 unit = 100 calories |
| B4152 | EF calorie dense>/=1.5Kcal | 1 unit = 100 calories |
| B4153 | EF hydrolyzed/amino acids | 1 unit = 100 calories |
| B4154 | EF spec metabolic noninherit | 1 unit = 100 calories |
| B4155 | EF incomplete/modular | 1 unit = 100 calories |
| B4157 | EF special metabolic inherit | 1 unit = 100 calories |
| B4158 | EF ped complete intact nut | 1 unit = 100 calories |
| B4159 | EF ped complete soy based | 1 unit = 100 calories |
| B4160 | EF ped caloric dense>/=0.7kc | 1 unit = 100 calories |
| B4161 | EF ped hydrolyzed/amino acid | 1 unit = 100 calories |
| B4162 | EF ped specmetabolic inherit | 1 unit = 100 calories |
Parenteral Nutrition Kits
B4220: Supply kit for pre-mix
B4222: Supply kit for home mix
B4224: Administration kit
Parenteral Nutrition Pumps
B9004: Parenteral nutrition infusion pump; portable
B9006: Parenteral nutrition infusion pump; stationary
Parenteral Nutrients
Parenteral nutrients are billed in grams of protein per bag/day and also per 10 grams of lipids.
| Parenteral Nutrient B-Codes | ||
| HCPCS Code | Description | Billing Unit/ Frequency |
| B4185 | Lipids. Fat emulsions | Per 10 GM |
| B4189 | 10-51 Grams of Protein | Per day |
| B4193 | 52-73 Grams of Protein | Per day |
| B4197 | 74-100 Grams of Protein | Per day |
| B4199 | Over 100 Grams of Protein | Per day |
Under the commercial per diem structure nursing visits are billable using the following codes:
99601 – Home infusion/specialty drug administration, per visit (up to 2 hrs.)
99602 – Home infusion/specialty drug administration, each additional hour
CPT codes 99601 and 99602 are used for high-tech RN services–provided by a RN with special education, training and expertise in home administration of drugs via infusion, home administration of specialty drugs, and/or home nursing management of disease state and care management programs.
Typical services include evaluation and assessment, education and training for the patient or caregiver, inspection and consultation of aseptic home environment, catheter insertion, and patient assessment.
To illustrate the CPT coding with a brief example, if total time required for all activities involved for a nurse visit is 2 hours and 40 minutes, coding is:
Medicare and Medical Assistance does not recognize 99601/99602. These codes are primarily billed for Commercial insurances.
Nursing Services – Medicare Part A Certified Home Health Agency (HHA)
G0162 – Skilled services by a registered nurse (RN) for management and evaluation of the plan of care; each 15 minutes (the patient’s underlying condition or complication requires an RN to ensure that essential non-skilled care achieves its purpose in the home health or hospice setting)
Medicare only allows for nursing services as part of a home health episode of care provided by a Part A licensed nursing agency. This often requires that home and specialty infusion pharmacy coordinate the nursing care through a 3rd party, who bills Medicare directly for the episode of care. There is a long list of criteria related to coverage of home health services and is the responsibility of the Part A certified home health agency to determine if the patient qualifies for nursing in the home.
Medicaid and Medicaid Managed Care Organizations coverage for nursing varies. Be sure to check the plan specific policy manuals for coding instructions. *Prior authorization may be required.
Medical vs. Pharmacy Benefit and “Split Billing”
A patient’s home infusion benefit may be split between the pharmacy (drug) and the major medical (supplies). This practice is known as split billing or bifurcated billing. This practice is prevalent when billing Medicaid which makes a distinction between the pharmacy benefit and the medical benefit. This is also commonly seen when billing specialty drug. Billers must understand the payer requirements to ensure the appropriate payer is billed.
Split billing requires that the drug is submitted to the PBM via an NCPDP claims and the service, supply and equipment portion is submitted on a CMS 1500 or electronic equivalent.
Conversely, when antibiotics are billed, the drug is always billed separately therefore if a patient is hospitalized, the provider may still be able to bill the drug and forgo the per diem.
Single dose vials (SDV): manufactures may classify their products as single dose vials which means they do not contain preservatives. The vial is not meant to be used for multiple entries (patients).
Multi dose vials (MDV): these are “bulk” vials and typically do contain preservatives. They can be entered multiple times. An example of a MDV of insulin. If refrigerated, insulin vials are kept up to 30 days. Likewise, there are bulk vials of antibiotics such as vancomycin. It is common for pharmacies to purchase 5GM or 10GM vials which can be used to make multiple IVs.
A payer’s wastage policy may be driven by the use of SDV and MDV. If a medication is only available as a SDV and the dose prescribed is less than the amount in the SDV there will be hood wastage. The provider may be permitted to bill for the contents of the entire vial. An example of this is a drug called daptomycin. It only comes in a 500 MG vial but a patient’s dose may be less than that amount. Due to the cost of this drug, it is beneficial to the provider to know whether they can bill for this hood wastage.
Regarding MDV wastage, payers may exclude billing for wastage or they may only allow it if the smallest size vial is used to compound the product. The antibiotic ceftriaxone come in several vial sizes from 250MG to 10GM. If a patient is prescribed a total of 4 GM and the pharmacy uses a 5GM vial to compound the prescription, they payer may not allow for hood wastage because there are smaller vial sizes available to include 1GM and 2 GM vials.
Another note is that if a payer does allow the provider to bill for drug wastage, they may require that that the amount wasted is reported on a separate line item using the JW modifier.
| Common Billing Modifiers | |||
| RR | Rental; placed in the first position and billed until the rental is capped/ownership is transferred to the patient | ||
| KH | First month of rental; placement after the RR modifier | ||
| KI | Second and third month of rental; placement after the RR modifier | ||
| KJ | Fourth through thirteenth month of rental; placement after the RR modifier | ||
| KD | B Covered drugs infused through DME; drug modifier; consult payer policy (not used by Medicare) | ||
| JB | Indicates subcutaneous infusion; use with syringe pump in addition to the rental and month modifier. (Example: RR KI JB) | ||
| JA | Administration intravenously (Not used by Medicare) | ||
| JW | Drug wastage; reported on a separate line. | ||
| GA | ABN on file | ||
| GY | Item or service statutorily excluded; NO ABN on file | ||
| GZ | Item or service expected to be denied as not reasonable and necessary | ||
| NU | Item that is new or has been purchased; use for disposable IV poles | ||
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |